Cervical Cancer Screening In Vietnamese Women
Cau Van Vo, MD., FACOG. |
||||||||||||||||||||
Epidemiology Approximately 13,000 new cases of Cervical Cancer and 4,600 deaths occur annually in the United States. The death rate from Cervical Cancer is about 3.0 per 100,000 women. This is the third most gynecologic cancer death in the United States. Incidence of Invasive Cervical Cancer The incidence of cervical cancer by rate: -White 8.1 per 100,000 women Risk Factors * Risk factors associated with precancerous changes and cancer of cervix -High risk human papilomavirus infection (HPV) * Other risk factors -20% of women in the United States do not undergo regular cervical cytology screening (Pap smear). * Additional specific risk factors in Vietnamese women Etiology A 1995 study in the Journal of the National Cancer Institute (JNCI) reported finding genetic material of oncogenic HPV in 93% of invasive cervical cancer. Disease course The progression to invasive cervical cancer is an important factor in the determination of cervical cytology screening. Over the last decade, it becomes clear that the beginning of infection with HPV is necessary for the development of high-grade lesions and cervical cancer. However, until 2001, it has been well established that cervical infection with high-risk HPV causes the majority of invasive cervical cancer. Mean transition time from mild to severe is approximately 5.8 years and from moderate to severe is approximately 3.1 years. Mean transition time from severe to invasive cancer is about 10 years. Revised Bethesda System Classification 2001 Satisfactory or unsatisfactory slides
|
||||||||||||||||||||
Pap smears should continue at least yearly in women with a history of in-utero DES exposure, HIV infection or immunosuppressant status. Continue screening if the patient is in reasonably good health without a life-limiting condition and cervical cytology was never performed. Continue screening if the previous cytology report is not available or there is a history of dysplasia, cervical cancer or HIV
Suggestion of Cervical cancer screening in Vietnamese women. Vietnamese women have the highest invasive cervical cancer rate in the United States of America. It is 5 times higher than white women. There are many factors; however, the main reason is still lack of regular gynecologic exam and annual cytologic screening. In our culture, women are not used to talking about sexual activities in public and letting other people see their intimate parts. That is the reason why many women are embarrassed to see their doctor for a pelvic exam and a Pap smear. Many Vietnamese women also believe as long as they do not have any symptoms they would have been healthy. Following are the guidelines recommended: |
||||||||||||||||||||
|
||||||||||||||||||||
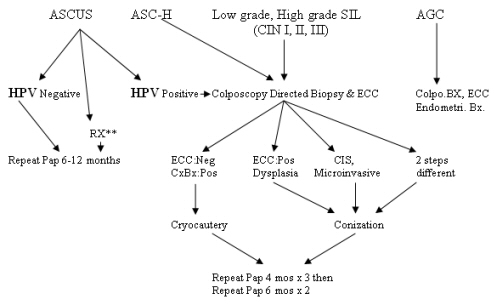
Management of Cervical Dysplasia |
||||||||||||||||||||
 |
||||||||||||||||||||
RX** Menopausal women who have cytological evidence of atrophy should be treated with intravaginal estrogen if there are no contraindications. |
||||||||||||||||||||
Conclusion. Cervical cancer screening is a very effective method to detect the precancerous stage that is easily treatable and the deadly cervical cancer can be prevented. Remember, most deaths from cervical cancer occur among women who have never had a Pap test. Vietnamese American women are still influenced deeply by our culture. Many women are embarrassed and timid to see their Gynecologist. This is the main reason of the highest cervical cancer rate in the United States. However, there are still other high-risk factors such as DES exposure, first pregnancy at early age, multiparity… Some studies show that the addition of HPV DNA testing to a cervical screening in women below 30 years of age will improve the sensitivity of detecting CIN I or greater about 95%. Even with this new combination of tests, some women will still develop invasive cancer. Improved screening technology is important, but encouraging every Vietnamese woman into a regular cervical cancer screening will still be the utmost important goal. Instead, Obstetricians and Gynecologists should adopt the guidelines and explain the important of a Pap test. We need to redouble our efforts to educate the Vietnamese women the value of an annual exam for other health assessments such as detecting ovarian cancer, screening breast cancer and recto-colon cancer, not cervical cancer screening alone. References |
||||||||||||||||||||
 |
||||||||||||||||||||

